Before medical device manufacturers can bring a device to market, they must first demonstrate its biocompatibility to the FDA. And from the FDA’s perspective, this is what the term means:
- Biocompatibility is the ability of a device to perform with an appropriate host response in a specific situation.
That’s from Use of International Standard ISO 10993-1, an FDA guidance document that details important concepts medical device manufacturers need to know about biocompatibility standards and testing.
Knowledge of these standards is essential in properly classifying, preparing, and submitting a medical device for FDA clearance or approval. In this guide, we’ll address the FDA’s approach to biocompatibility and what MDMs must provide to regulators to pass their device through 510k clearance or premarket approval.
Expanding on the FDA’s Definition of Biocompatibility
According to the FDA’s own definition, biocompatibility is a relative term that considers the device’s mechanical, chemical and structural properties, as well as how those properties interact with the host.
To boil it down further – a biocompatible device is a device that performs its intended function without producing toxic effects in the host.
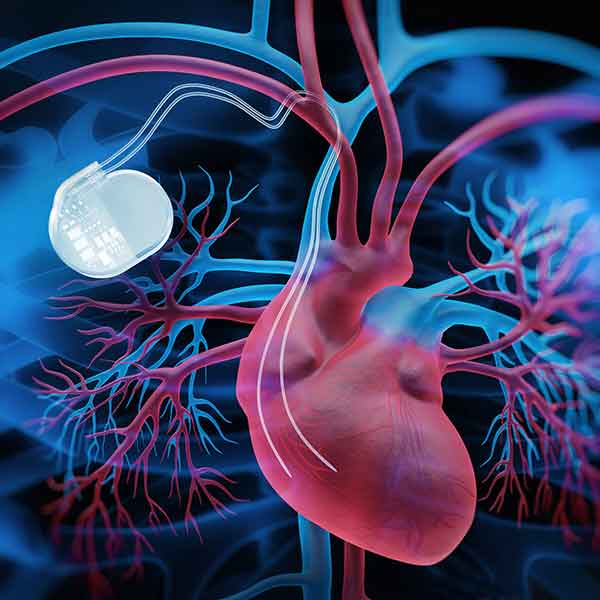
Using this definition, the device’s intended function leads the biocompatibility discussion. A catheter intended for cardiac catheterization, for example, must remain in contact with the patient’s blood without causing toxicity. By contrast, a dermal patch is considered biocompatible as long as it’s safe to use with the patient’s skin.
As such, assessing biocompatibility is a device-by-device process.
Verifying Biocompatibility is an Important Part of the FDA’s Regulatory Process
The FDA requires biocompatibility evaluations for any medical device that comes in direct or indirect contact with the human body. Exactly what those evaluations should include depends on the following:
- The duration of contact
- The tissues the device will contact
- The device’s potential risks
That last bullet is of particular importance. The FDA requires MDMs to subject their devices to a comprehensive risk assessment – the goal being to identify where potential risks could emerge and what information must be produced to ensure those risks are mitigated.
What Must a Biocompatibility Risk Assessment Include?
During risk assessment, MDMs must consider the properties of the final product. The FDA does not approve or clear constituent materials that make up a medical device – only the final device itself. This means device manufacturers must base their risk assessment on final device samples.
As for the assessment, some of the potential risks may include:
- Chemical toxicity
- The device’s physical geometry
- Mechanical, electromagnetic or thermal forces applied to tissues
- The device’s surface properties
- Manufacturing and processing parameters
Risk assessments must take the intended clinical use and patient population into context, as well. If the device is intended for patients with low life expectancy, for example, risk tolerance may be higher than it would be in a healthy patient population. When establishing biocompatibility endpoint for risk assessment and testing purposes, the FDA may approve devices that have potential risks, but provide medical benefits that outweigh those risks.
Once all potential risks are identified, MDMs may either devise testing methods that quantify them, or use predicate devices to establish biocompatibility equivalence.
Using Equivalence to Establish Biocompatibility
For more than a decade, the FDA has looked to the ISO 10993-1 standard for guidance on establishing appropriate biocompatibility endpoints, as well as how to test for those endpoints.
The ISO 10993-1 standard, as well as the FDA, encourage medical device manufacturers to consult the available research literature prior to devising biocompatibility testing measures. By doing so, MDMs may be able to use predicate devices or materials to show that their own device design and composition is safe. It’s a similar concept to using a predicate device to attain 510k clearance – a process we’ve detailed here.
The FDA’s definition of equivalence covers several aspects of device design. For example, when the FDA refers to equivalence, they’re describing one or more of the following:
- Contact equivalence – If the intended clinical use for two devices or materials is sufficiently similar, they are considered to have contact equivalence.
- Chemical equivalence – If two materials or devices are chemically similar, to the point where chemical composition or device processing do not produce additional toxicological risks, those devices possess chemical equivalence.
- Physical equivalence – If two materials or devices are sufficiently similar in morphology, topography, configuration and tribology, they are considered physically equivalent.
- Material equivalence – If two materials or devices are physically and chemically equivalent, they are considered materially equivalent as well.
- Biological equivalence – If two devices possess contact and material equivalence, they are considered biologically equivalent by the FDA.
If all of the above can be demonstrated using existing data sheets, clinical studies and research, then additional biocompatibility testing may not be required. If there are any existing “knowledge gaps” (the FDA’s term) even after reviewing the existing medical literature, biocompatibility testing will be required.
Using Testing to Establish Biocompatibility
Again, the required biocompatibility testing for a particular device depends on what tissues it will contact and how long it will contact those tissues. For example, implantable devices that contact blood must satisfy the following biocompatibility endpoints:
- Cytotoxicity
- Sensitization
- Irritation
- Acute, subchronic, and chronic systemic toxicity
- Genotoxicity
- Material mediated pyrogenicity
- Hemocompatibility
- Carcinogenicity
- Implantation
The FDA has developed detailed test considerations to guide MDMs in developing the above testing methods. This information is available in the FDA’s Use of International Standard ISO 10993-1 document.
According to the same document, the FDA encourages device manufacturers to pursue in vitro testing instead of in vivo testing when possible. The reason being to minimize the number of living animal subjects used for medical research purposes. For many biocompatibility endpoints, in vitro testing produces information that’s sufficiently similar to in vivo tests.
Use of International Standard ISO 10993-1 also includes guidelines on test sample preparation. Notable points include:
- When possible, the amount of test sample should be based on the device’s surface area, and not mass. Mass-to-extract-volume ratios are only acceptable if the device’s surface area cannot be calculated for this purpose.
- Mixed polarity solvents must be used when identifying potential extractables. This ensures both hydrophilic and lipophilic chemicals are detected during testing.
- Test samples must not be subjected to any processing methods that the final sample will not be subjected to. This includes filtration and centrifugation.
- Test samples must be used within a timeframe specified by ISO 10993-12. If stored past this timeframe, the device manufacturer must demonstrate storage will not affect the device’s biocompatibility.
Using the above testing standards and guidelines, MDMs can produce data that fills any remaining knowledge gaps and demonstrates how potential risks are mitigated by the device’s design or composition.
An Experienced Medical Plastics Converter Can Support an MDM’s Efforts to Demonstrate Device Biocompatibility
The device’s material composition, chemical composition and physical design are all primary biocompatibility considerations. For MDMs designing products in PEEK, Radel or other medical grade plastics, a polymer converter experienced in stock shapes extrusion, injection molding or film calendering can help establish the necessary biocompatibility endpoints.

A specialist in calendering implantable grade PEEK film, for example, can provide detailed data on material composition, chemical composition, processing methods, manufacturing procedures and quality systems. This information can be developed so that it is comprehensive enough for an FDA review of an MDM’s implantable device utilizing the PEEK film. It can also be organized to meet the agency’s formatting standards.
Establishing biocompatibility is a mandatory hurdle that most MDMs must clear before their device can be marketed. The process is complex and time-consuming, but it’s made much easier with the expertise and insight that an expert medical polymer converter offers.
